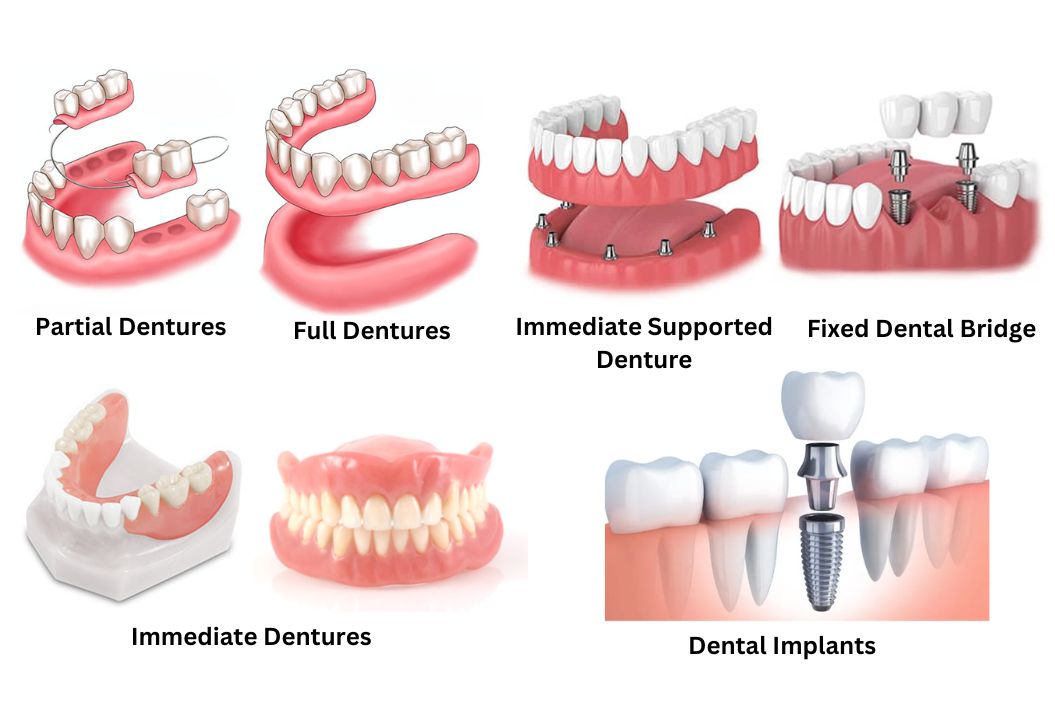
Exploring the Diverse World of Dentures
Losing natural teeth no longer means sacrificing function or appearance. Advances in dental prosthetics have created a wide range of solutions that restore chewing efficiency, speech clarity, and facial support. Understanding how different denture designs work helps patients make informed, long-term oral health decisions.
The Role of Dentures in Oral Rehabilitation
Restoring Function and Facial Structure
When teeth are lost, the jawbone gradually resorbs due to lack of stimulation, which can alter facial contours and lead to a collapsed appearance. Dentures help distribute occlusal forces during chewing, supporting facial muscles and improving masticatory function. Properly fitted prostheses can also enhance phonetics by stabilizing tongue and lip movements during speech.
Materials and Fabrication Techniques
Full Dentures and Their Clinical Applications
Conventional Full Dentures
Immediate Dentures
Partial Dentures for Targeted Tooth Replacement
Traditional Partial Dentures
Flexible Partial Dentures
Implant-Supported Dentures and Overdentures
Implant-Supported Dentures
Overdentures
| Denture Approach | Stability Level | Maintenance Considerations | Typical User Profile |
|---|---|---|---|
| Conventional removable dentures | Moderate | Regular adjustments and relining | Patients seeking non-surgical solutions |
| Implant-Supported Dentures | High | Implant hygiene and periodic evaluations | Patients prioritizing stability and function |
| Overdentures | High to very high | Attachment maintenance | Patients balancing removability with support |
Clinical Considerations When Choosing Denture Types
Oral Health and Bone Condition
Lifestyle and Adaptation Factors
| Decision Factor | Why It Matters | Denture Types Commonly Considered |
|---|---|---|
| Bone support | Determines feasibility of implants | Implant-Supported Dentures, Overdentures |
| Aesthetic expectations | Influences material and design | Flexible Partial Dentures, Full Dentures |
| Manual dexterity | Affects ability to remove and clean | Fixed or semi-removable options |
| Long-term maintenance | Impacts follow-up frequency | All denture categories |
Long-Term Care and Maintenance of Dentures
Daily Cleaning and Hygiene
Professional Follow-Up and Adjustments
Q&A
-
What are Full Dentures best suited for?
Full Dentures are most appropriate for individuals who have lost all natural teeth in one or both arches. They restore basic chewing function, support facial structure, and improve speech when properly designed and adjusted.
-
How do Partial Dentures differ from Flexible Partial Dentures?
Traditional partial dentures often use metal frameworks and clasps, while Flexible Partial Dentures rely on thermoplastic materials. The flexible option typically offers improved comfort and aesthetics but may not provide the same level of rigidity for certain bite conditions.
-
Are Immediate Dentures a permanent solution?
Immediate Dentures are usually considered a transitional option. As healing progresses and tissue contours change, they often require relining or replacement with a definitive prosthesis for long-term use.
-
What advantages do Implant-Supported Dentures provide?
Implant-Supported Dentures offer superior stability, improved chewing efficiency, and reduced bone resorption compared to tissue-supported dentures. They are particularly beneficial for patients who struggle with denture movement.
-
How are Overdentures different from fixed implant prostheses?
Overdentures are removable and attach to implants or retained roots using specialized connectors. This design allows for easier cleaning while still providing enhanced stability compared to conventional removable dentures.
