Unveiling the Hidden Connections: Oral Pain and Systemic Health
The subtle interplay between overall well-being and aches in the oral cavity often goes unnoticed. With roots beyond our daily comprehension, these discomforts serve as vital indicators of broader health dynamics, revealing the interconnectedness of various bodily systems through unexpected pathways.
The Circulatory and Metabolic Loop
When Blood Sugar Disrupts the Barrier
We often think of cavities and gum issues as a result of skipping a brushing session or indulging in too many sweets. However, persistent gum sensitivity and inflammation can sometimes signal a deeper metabolic disruption. For individuals navigating the complexities of regulating blood glucose, the oral environment transforms significantly. Elevated sugar levels are not just present in the blood; they manifest in saliva as well. This creates a feast for naturally occurring oral bacteria, allowing them to multiply at an accelerated rate.
The relationship here is a frustrating two-way street. Not only does uncontrolled glucose encourage bacterial overgrowth leading to periodontal challenges, but active gum infection also makes it physically harder for the body to manage blood sugar levels. The inflammation in the gums releases chemical signals into the bloodstream that increase insulin resistance. This creates a cycle where oral pain is both a symptom and a contributor to the metabolic condition. Recognizing that red, swollen, or bleeding gums might be a flag for checking insulin levels is a crucial step in holistic health management. It shifts the perspective from "I need a better toothpaste" to "I need to check my body's chemical balance."
The Inflammatory Pathway to the Heart
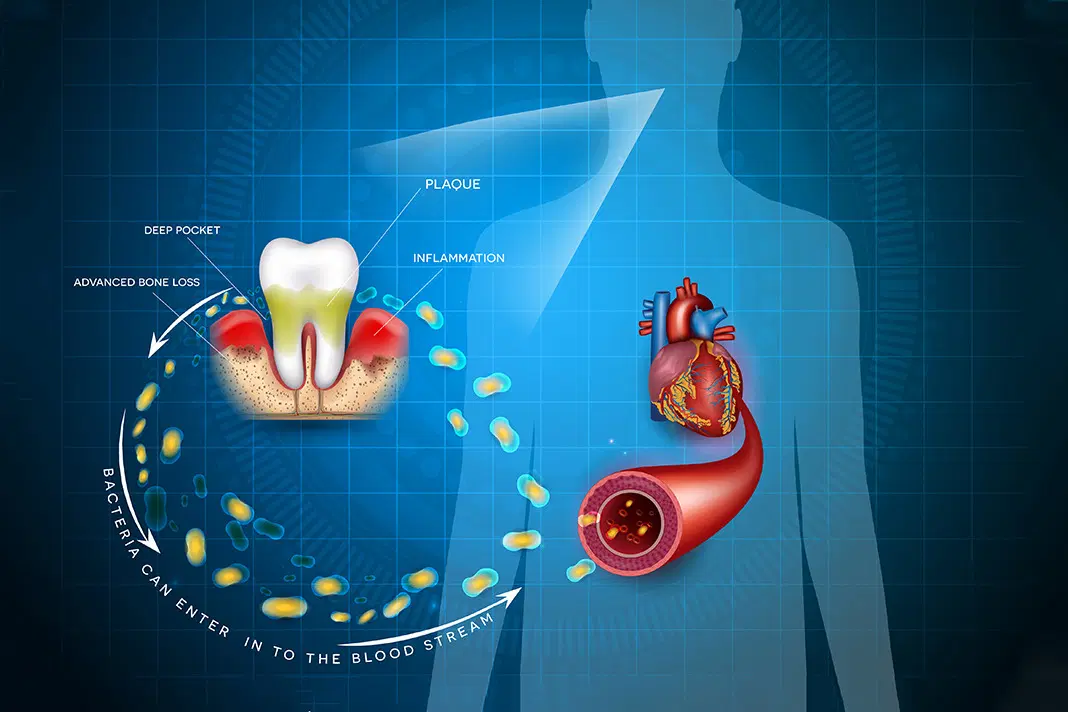
The concept that the mouth is a mirror to the body is perhaps most critical when discussing heart health. Modern science has begun to map out how oral bacteria, specifically those thriving in deep gum pockets, do not stay confined to the mouth. When gum tissues are compromised and bleed, these bacteria can enter the bloodstream, traveling far from their point of origin.
Once in the circulatory system, these pathogens can attach to fatty plaques in the coronary arteries, potentially contributing to clot formation. However, the more significant link is inflammation. Chronic infection in the mouth keeps the body's immune system on high alert, elevating inflammatory markers like C-reactive protein. High levels of generalized inflammation are a known risk factor for cardiovascular events. Therefore, treating oral pain and eliminating infection isn't just about saving a tooth; it is an active measure of protecting the intricate network of veins and arteries that power the body.
Hormonal Tides and Immune Resilience
The Sensitivity of Expecting Mothers
During pregnancy, the body undergoes a seismic shift in hormonal balance, particularly with surges in progesterone and estrogen. These hormonal changes dramatically affect the blood vessels in the gums, making them more permeable and susceptible to the effects of plaque bacteria. Many women experience what is colloquially known as "pregnancy gingivitis," where gums become tender, swollen, and bleed easily, even with excellent hygiene.
This reaction is the body's exaggerated response to irritants that it would normally tolerate. In some cases, localized swellings or benign growths can appear between teeth, often vanishing after childbirth. It is a vivid reminder that the mouth is not an isolated ecosystem but a reactive part of the body's endocrine system. Managing this sensitivity requires a delicate balance—maintaining rigorous hygiene without traumatizing the sensitive tissues. Ignoring these symptoms is ill-advised, as active infections during this critical period have been theoretically linked to broader complications. Thus, oral tenderness during these nine months is less about the teeth and more about the hormonal narrative playing out internally.
Signals from a Compromised Defense System
The lining of the mouth acts as a primary barrier and a frontline scout for the immune system. When the body’s natural defenses are weakened—whether due to fatigue, stress, or specific medical conditions—the oral cavity is often the first place to show signs of distress. Microorganisms that are typically harmless can suddenly seize the opportunity to grow unchecked.
We often see this manifest as fungal infections, such as thrush, or painful ulcers that refuse to heal. Unlike the common canker sore caused by biting one's cheek, these lesions can be widespread and persistent. They serve as a biological "check engine" light, warning that the immune surveillance is down. For individuals managing autoimmune conditions, the mouth can develop specific patterns of inflammation, such as lace-like white patches or desquamation of the gums. These are not merely dental annoyances; they are visible readouts of the immune system's current capacity. Recognizing these signs allows for early intervention, boosting the body's defenses before a systemic infection takes hold.
External Influences and Vigilance
The Impact of Pharmacological Treatments
In our modern medical landscape, many individuals rely on daily medications to manage everything from mood to blood pressure. While these drugs are life-saving, a vast number of them share a common, often overlooked side effect: the reduction of salivary flow. Saliva is the unsung hero of oral health; it neutralizes acids, washes away food particles, and contains enzymes that digest starch.
When medication suppresses saliva production, the protective buffer is lost. This condition, known clinically as xerostomia, leads to a rapid increase in tooth decay and a burning sensation in the soft tissues. It is not simply a matter of feeling thirsty; the lack of lubrication causes friction against the tongue and cheeks, leading to chronic pain and difficulty swallowing. Patients often blame their age or diet, not realizing the capsule they take with breakfast is the culprit. Understanding this link is vital for patients to discuss alternatives or management strategies with their physicians, ensuring that treating one condition doesn't ruin their oral ecosystem.
The Importance of Monitoring Cellular Changes
One of the most serious aspects of oral health is the potential for tissues to undergo cellular changes. Unlike teeth, which are hard structures, the soft lining of the mouth is constantly regenerating. Sometimes, due to genetic factors or lifestyle habits, the regeneration process goes awry. This is where the concept of screening becomes a lifesaver.
Early stages of dangerous cellular mutations often do not cause pain. They manifest as subtle color changes—patches of red or white—or small lumps that feel different from the surrounding tissue. By the time pain is present, the condition may have advanced significantly. Therefore, being vigilant about "silent" changes is just as important as reacting to a toothache. Regular examinations are not just about finding cavities; they are a comprehensive scan for irregularities in the soft tissue. If a sore or a patch persists for more than two weeks without a clear cause (like a pizza burn or a bitten lip), it warrants professional evaluation. This proactive approach transforms dental visits from a chore into a critical component of preventative medicine.
Q&A
-
What is the correlation between cardiovascular disease and oral health?
Cardiovascular disease has been linked to oral health, specifically periodontal disease. Inflammation caused by gum disease can contribute to the development of atherosclerosis, a condition characterized by the hardening of the arteries, which can lead to heart attacks or strokes. Maintaining good oral hygiene can potentially reduce the risk of cardiovascular issues.
-
How does diabetes affect periodontal health?
Diabetes-related periodontitis is a concern because high blood sugar levels can lead to increased inflammation and vulnerability to infections, including those in the gums. Poorly managed diabetes can exacerbate periodontal disease, and conversely, severe periodontitis can make it more difficult to control blood sugar levels, creating a cyclical problem.
-
What are the oral health risks for immunocompromised individuals?
Immunocompromised individuals are at higher risk for oral infections and conditions such as fungal infections, viral lesions, and periodontal disease due to their weakened immune system. It's crucial for these individuals to maintain rigorous oral hygiene and have regular dental check-ups to prevent complications.
-
What causes pregnancy gingivitis and how can it be managed?
Pregnancy gingivitis is caused by hormonal changes during pregnancy that increase blood flow to the gums and alter the body's response to plaque. This can lead to swelling, bleeding, and tenderness of the gums. Pregnant women can manage this condition by maintaining good oral hygiene, using a soft-bristled toothbrush, and visiting a dentist regularly for cleanings.
-
How does medication-induced xerostomia affect oral health, and what can be done to alleviate it?
Medication-induced xerostomia, or dry mouth, occurs when certain medications reduce saliva production. This can lead to difficulties in speaking, eating, and an increased risk of cavities and oral infections. To alleviate dry mouth, individuals can increase their water intake, chew sugar-free gum to stimulate saliva flow, and use saliva substitutes or oral moisturizers. Regular dental visits are also recommended to monitor and manage oral health.
