How Seasonal Allergies Intensify Maxillary Sinusitis and Dental Pain
As the changing seasons cast their influence, the interplay between environmental factors and bodily responses can manifest in unexpected discomfort. This intricate relationship may lead to a puzzling blend of facial unease and dental irritations. Understanding these connections becomes key to alleviating persistent pain and discomfort.
The Anatomical Crossroads of Nose and Mouth
The Thin Barrier Between Respiratory and Dental Systems
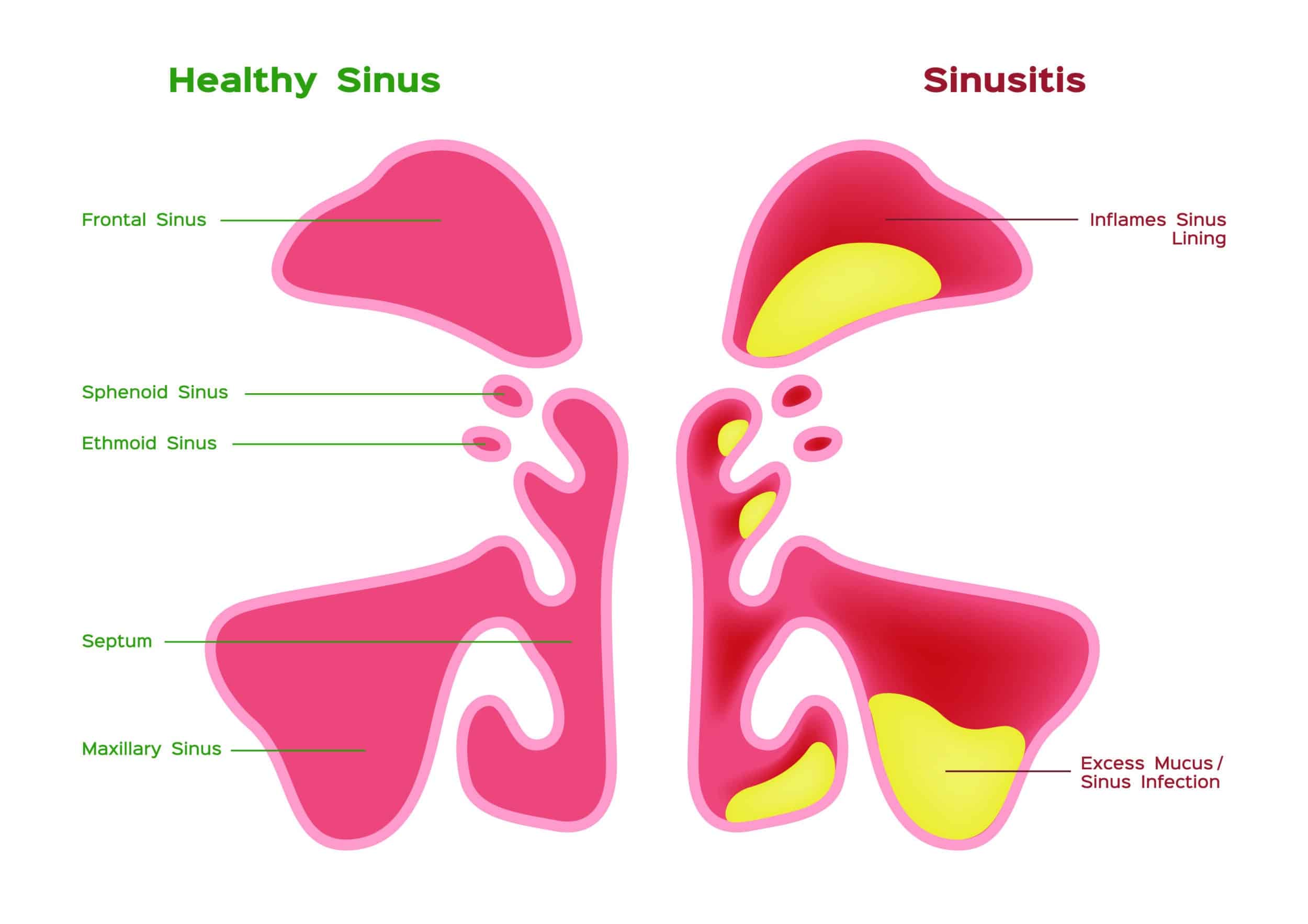
It is a common misconception that our oral health and respiratory systems operate in complete isolation. However, deep within the facial structure, there exists a biological intersection that often confuses patients and complicates diagnoses. The maxillary sinuses, which are large, air-filled cavities located behind your cheekbones and on either side of your nose, sit directly atop the upper jaw. The anatomical reality is that the floor of these sinus cavities and the roots of the upper back teeth—specifically the molars and premolars—are neighbors separated by an incredibly thin layer of bone. In some individuals, this bone is paper-thin, or the tooth roots may even protrude slightly into the sinus cavity, covered only by a delicate mucous membrane.
When this membrane becomes inflamed due to a cold, infection, or environmental irritants, the tissue swells significantly. Because the sinus cavity is a rigid bony box, the swelling has nowhere to go but inward, filling the empty space and exerting force against the walls. This creates a high-pressure environment right next to the sensitive nerve endings of the tooth roots. Consequently, the inflammation in the nose transmits distress signals directly to the teeth. You might feel a sensation that mimics a severe cavity or a dying nerve, yet the tooth itself is structurally sound. This phenomenon explains why a person might rush to the dentist complaining of excruciating pain, only to be told that their X-rays look perfect. The issue lies not in the tooth, but in the "attic" directly above it. Understanding this anatomical intimacy is the first step in realizing that not all toothaches originate from the teeth themselves.
| Feature | Dental Origin (Cavity/Infection) | Sinus Origin (Inflammation/Pressure) |
|---|---|---|
| Pain Localization | Usually sharp and confined to a specific, single tooth. | Often a dull ache affecting several upper back teeth simultaneously. |
| Temperature Sensitivity | Sharp, lingering pain when consuming hot or cold items. | Generally mild or non-existent; pain is more about pressure. |
| Effect of Movement | Movement rarely changes the intensity of the pain. | Pain throbs or worsens when bending over, walking heavily, or jumping. |
| Visible Signs | Swelling of the gum, dark spots on teeth, or holes. | No visible dental changes; often accompanied by nasal discharge or congestion. |
Deciphering the Signals of Discomfort
recognizing the nuances of pressure-based pain
Differentiating between a true dental emergency and referred pain from the sinuses requires paying close attention to the specific qualities of the discomfort. Unlike the sharp, piercing zap of an exposed nerve caused by decay, pain stemming from sinus issues tends to be heavier, duller, and more expansive. It often feels like a deep ache that radiates across the entire cheekbone or affects a row of teeth rather than a single point. A key indicator is the "movement test." Because the pain is driven by fluid dynamics and pressure within the head, changing your physical orientation often changes the pain level.
For instance, simple actions like tying your shoelaces, picking an object off the floor, or even lying down flat can cause blood and fluid to rush to the inflamed area, instantly increasing the throbbing sensation in the teeth. Similarly, the impact from walking down stairs or jogging can send a jolt through the upper jaw. This is known as "step-sensitivity." If you can reproduce the tooth pain by stomping your foot or shaking your head, the culprit is likely located above the teeth, not within them. This mechanical sensitivity occurs because the inflamed tissues and accumulated fluids in the sinus cavity are physically pressing against the superior alveolar nerves that supply sensation to the teeth.
Furthermore, this type of discomfort often fluctuates with the time of day or environmental conditions. You might wake up with significant pain that eases as you move around and the sinuses drain, or you might notice the pain intensifies when you enter a dry, air-conditioned room that irritates the nasal lining. Recognizing these patterns is crucial. Many patients endure root canals or extractions they didn't need, simply because the source of the pressure was misunderstood. If the pain is bilateral—meaning it is felt on both the left and right sides of the upper jaw simultaneously—it is almost certainly a sinus-related event, as it is statistically improbable for teeth on opposite sides of the mouth to develop identical decay at the exact same moment.
The Seasonal and Environmental Connection
How Allergies Fuel the Cycle of Inflammation
For many sufferers, the bridge between nasal congestion and tooth pain is built by seasonal changes. When spring arrives with high pollen counts, or winter brings dry air and dust mites, the body's immune response kicks into high gear. Allergic rhinitis is not just about sneezing; it triggers a cascade of inflammation that causes the mucous membranes lining the nose and sinuses to thicken rapidly. This swelling blocks the ostium—the tiny drainage hole that allows the sinus to ventilate. Once this exit is blocked, mucus gets trapped, creating a stagnant environment perfect for bacterial growth and pressure buildup.
This "chain reaction" of inflammation implies that treating the tooth pain with standard painkillers is often ineffective because it doesn't address the root cause: the allergic response. The pressure building up in the blocked sinus cavity acts like a balloon inflating inside the cheekbone, compressing the nerves mentioned earlier. Moreover, recent insights suggest that the immune response itself releases specific chemical mediators that can lower the pain threshold of the nerves in the surrounding area, making the teeth feel hypersensitive even before significant pressure builds up. This creates a state of hyper-alertness in the facial nerves, where even minor stimuli feel painful.
Effective management requires a two-pronged approach. Ignoring the nasal symptoms to focus solely on the teeth will lead to frustration, while ignoring the dental symptoms to focus only on the allergy might miss a coincidental dental infection. The goal is to reduce the inflammatory load. This often involves lifestyle adjustments to minimize allergen exposure, such as using air purifiers or saline rinses to mechanically remove irritants from the nasal passages. By reducing the swelling in the sinus lining, the pressure on the dental nerves is relieved, and the "toothache" often vanishes as if by magic. It is a reminder that the body is a unified system; clearing the air passages is frequently the most effective form of dental pain relief during allergy season.
| Symptom Scenario | Suggested Primary Focus |
|---|---|
| Pain usually upon waking, improves during the day | Drainage Management: Focus on sleeping position and nighttime humidity levels to prevent congestion buildup. |
| Pain triggered by cold air or specific seasons | Allergen Control: Prioritize reducing exposure to environmental triggers like pollen or dry air. |
| Pain accompanied by fever or yellow/green discharge | Infection Control: This suggests a bacterial infection requiring medical assessment beyond simple allergy care. |
| Persistent pain despite clear nasal passages | Dental Assessment: If sinus pressure is ruled out, a thorough dental exam is necessary to check for cracks or decay. |
Q&A
-
What is referred toothache and how is it connected to sinus issues?
Referred toothache occurs when pain is felt in the teeth but originates from another source, such as the sinuses. This can happen when the sinus floor is in close proximity to the roots of the upper teeth. Inflammation or pressure in the sinuses, often due to conditions like sinusitis or allergies, can create sensations of tooth pain.
-
How does antral pressure contribute to nasal congestion?
Antral pressure refers to pressure within the sinus cavities. Increased antral pressure can lead to nasal congestion as it affects the mucous membranes lining the nasal passages. This pressure can block the normal drainage pathways, causing mucus build-up and a sensation of fullness or congestion in the nose.
-
Why might seasonal allergies cause bilateral sensitivity in the sinuses?
Seasonal allergies, such as hay fever, often lead to inflammation of the nasal passages and sinuses on both sides of the face, known as bilateral sensitivity. Allergens like pollen trigger the immune system to release histamines, causing swelling and irritation in the sinuses and nasal passages, leading to bilateral discomfort and sensitivity.
-
What is the significance of sinus floor proximity to dental health?
The proximity of the sinus floor to the upper teeth can have significant implications for dental health. When the sinus floor is close to the roots of the teeth, sinus infections or inflammation can manifest as dental pain. Additionally, dental procedures near the upper teeth can inadvertently affect the sinus cavity, leading to complications such as sinusitis.
-
How can individuals manage symptoms related to sinus-induced toothache and nasal congestion?
Managing symptoms related to sinus-induced toothache and nasal congestion involves addressing the underlying sinus issues. This can include the use of decongestants, antihistamines, and nasal saline rinses to reduce congestion and inflammation. In cases of bacterial sinus infections, antibiotics may be prescribed. Avoiding known allergens and using air purifiers can also help minimize allergy-related symptoms.
